Millions of Americans still struggle to get the medications their clinicians prescribe. Even when treatment is urgent, patients face administrative delays, unclear coverage rules, benefit investigations, and unpredictable out-of-pocket costs. These barriers delay care, disrupt continuity, and worsen outcomes for patients managing chronic or time-sensitive conditions.
Direct-to-patient (DTP) dispensing reduces access friction by unifying prescribing, coverage checks, affordability support, fulfillment, and home delivery into one coordinated process. This streamlined model ensures each patient is matched with the most accessible and affordable pathway from the start.
Key Takeaways |
|---|
|
The Challenge with Traditional Pharmacy Workflows
Traditional pharmacy channels weren’t designed for the growing complexity of today’s specialty medications. Patients often face immediate friction from prior authorizations, benefit investigations, and repeated coordination among prescribers, payers, and external specialty pharmacies, all of which slow therapy initiation.
Research from the Journal of Managed Care & Specialty Pharmacy shows that when specialty prescriptions are transferred to external pharmacies, patients experience an average delay of six days extra before starting treatment. For conditions such as HIV, rheumatoid arthritis, or cancer, these delays can meaningfully impact clinical outcomes.
These access barriers compound quickly. Administrative workload remains a top challenge, with 95% of providers reporting difficulty initiating specialty therapies due to extensive authorization and coordination requirements. When combined with fragmented communication and inconsistent visibility into coverage status, the traditional system creates avoidable delays that directly affect whether patients begin treatment on time.
Cost Unpredictability Drives Prescription Abandonment
Unpredictable costs remain one of the strongest drivers of therapy abandonment. Patients often have no visibility into their final out-of-pocket amount until they reach the pharmacy counter, where unexpected charges can derail the entire treatment plan. Research highlights the impact of cost opacity:
42% of Americans struggle to afford their prescribed medications.
29% of adults are not taking medications as prescribed due to cost concerns.
Nearly 50% abandon therapy when out-of-pocket costs exceed $125.
These patterns show how quickly financial uncertainty, rather than clinical need, disrupts treatment. When patients cannot anticipate what they will owe, they are more likely to walk away from therapies that could improve their health.
How DTP Dispensing Simplifies Medication Access
DTP dispensing simplifies the entire prescription journey by consolidating all steps into a single, coordinated, patient-centered flow. Instead of dealing with multiple stakeholders, patients move through a unified process that brings together intake, coverage checks, benefit verification, fulfillment, and direct delivery.
By reducing handoffs and centralizing communication, DTP dispensing removes common access barriers and creates a smoother, more predictable experience from prescription to treatment.
Integrated Benefit Verification & Prior Authorization
Automated benefit verification (BV) and prior authorization (PA) are central to DTP dispensing's approach to removing early access barriers. The moment a prescription enters the system, automated checks identify coverage requirements and surface potential issues upfront, reducing the back-and-forth that commonly slows therapy initiation.
Key advantages of integrated BV & PA include:
Early issue detection, the moment a prescription arrives
Faster BV/PA turnaround times compared to external specialty pharmacies.
Higher approval rates due to coordinated, in-house processing
Less friction from fewer handoffs and communication gaps
By consolidating these steps into one workflow, DTP dispensing ensures patients move to fulfillment without avoidable delays. A study from the University of Kentucky HealthCare’s in-house specialty pharmacy found that patients received their specialty medications faster when processed through the health system’s integrated specialty pharmacy than through external specialty pharmacies.
Faster access supports better clinical care and reflects the value of keeping BV, insurance coordination, financial support and fulfillment within a single, patient-centered model; an approach DTP dispensing is designed to deliver.
Patient-Centered Telehealth & Medication Access
After coverage is confirmed, licensed pharmacists or pharmacy technicians engage patients via secure video or messaging to review medications, answer questions and verify dosing. These virtual check‑ins ensure that patients get counseling up front, rather than only at the point of delivery.
Once therapy is verified, DTP programs offer multiple fulfillment options. Medications can be shipped directly to a patient’s home, delivered to a trusted pick‑up site (e.g. a Walmart pharmacy or local clinic) or held at a designated community location to align with the patient’s schedule. This flexibility is crucial for people who live in “pharmacy deserts”. Approximately 1 in 7 Americans lack convenient access to a pharmacy, while some reports estimate that over 100 million people do not have reliable pharmacy access.
By coupling telehealth interactions with varied fulfillment options, DTP programs help overcome mobility, geographic and scheduling barriers. Remote consultations and direct shipping reduce the need for in‑person pharmacy visits, which is especially important as pharmacy closures and staff shortages have created deserts in rural and underserved communities.
Expanding Patient Choice Across Multiple Pathways
Instead of limiting patients to a single coverage channel, DTP creates flexibility across insurance benefits, cash-pay drug access, manufacturer affordability programs and emerging specialty affordability pathways. This combination of choice and upfront transparency reduces abandonment and ensures patients always have a clear route to obtain their medications.
Insurance Benefit Pathways
For patients using commercial or government insurance, DTP dispensing optimizes the benefit pathway by:
Checking coverage and formulary status in real time
Applying copay assistance when eligible
Providing upfront cost transparency to prevent surprise bills
Confirming the final out-of-pocket cost before needing to pay for the medication
This transparency also prevents the "surprise bill" scenario that drives so many patients to abandon prescriptions. When patients know what they'll owe upfront, they can make informed decisions about their care and plan accordingly.
Cash-Pay Drug Access
Not all patients have insurance coverage for their medications, and some prefer not to use it even in cases that they do. Some therapies aren't considered medically necessary by payers. Others fall outside formulary restrictions. And for certain medications, particularly those supporting weight management or cosmetic goals, insurance coverage may not exist.
DTP cash-pay programs provide an alternative pathway for these patients. Through manufacturer-sponsored programs and direct-to-consumer models, patients can purchase medications at predetermined prices without navigating insurance complexities.
These programs are paid directly by patients through online credit card processing. The model works particularly well for non-complex medications where diagnosis can be done virtually, allowing patients to access treatments remotely without the overhead of traditional pharmacy channels.
Manufacturer Affordability Programs
Pharmaceutical manufacturers have invested heavily in patient affordability programs that reduce out-of-pocket costs. These include copay assistance cards for commercially insured patients, patient assistance programs (PAPs) for uninsured or underinsured individuals, and bridge programs that provide temporary medication access while patients establish coverage.
DTP dispensing models integrate seamlessly with these affordability pathways. When a patient's coverage leaves them facing high out-of-pocket costs, the system can automatically surface applicable manufacturer programs and apply savings at the point of dispensing.
According to industry data, copay assistance programs are available at approximately 50,000 pharmacies nationwide, and automated applications help reduce prescription abandonment and improve therapy initiation. By embedding these programs directly into the DTP workflow, patients benefit without having to navigate complex enrollment processes.
MFN Pricing and Emerging Affordability Initiatives
Recent policy developments have created additional pathways to medication affordability. The Most Favored Nation (MFN) pricing initiative aims to align U.S. drug prices with those in comparable developed nations, potentially delivering significant savings for American patients.
Several major pharmaceutical manufacturers have announced agreements supporting MFN pricing through direct-to-consumer channels. These arrangements allow patients to purchase medications at reduced prices. In some cases, discounts reaching 80% or more off list prices - through dedicated purchasing platforms.
DTP dispensing provides the infrastructure to deliver these savings directly to patients. By controlling the distribution channel, manufacturers can pass meaningful cost reductions to consumers while maintaining product integrity and proper handling requirements.
Supporting Patients Who Struggle with Traditional Workflows
DTP dispensing is designed not only for efficiency, but also to support patients who routinely fall through the cracks of traditional pharmacy systems. By reducing complexity and offering guided support, DTP ensures that underserved, vulnerable or high-need patients can access and stay on therapy without the overwhelm of navigating fragmented workflows.
Patients Facing Administrative Barriers
Many patients cannot manage complex insurance requirements, multi-step PAs or enrollment processes. Limited health literacy, language barriers, physical limitations and cognitive challenges make traditional pharmacy pathways especially difficult.
DTP dispensing provides high-touch, guided support that helps patients:
Navigate insurance requirements
Manage PA requests
Access patient assistance programs (PAPs)
Coordinate refills and delivery.
This hands-on model ensures patients receive the support needed to move from prescription to treatment without being overwhelmed by administrative demands.
Patients with Unpredictable or Inadequate Coverage
Coverage often changes unexpectedly after job transitions, benefit exhaustion, insurance lapses, or formulary exclusions. Traditional pharmacies struggle to adapt quickly, leaving patients vulnerable to therapy interruptions.
DTP dispensing allows seamless pivots between:
Insurance benefit pathways
Cash-pay drug access
PAPs and bridge programs
By automatically identifying alternative pathways when coverage changes, DTP prevents treatment gaps and maintains continuity of care for chronic and progressive conditions.
Patients Managing Complex or Sensitive Conditions
Some conditions require enhanced privacy, specialized handling, or additional clinical oversight. Patients managing HIV, hepatitis C, fertility treatments, or oncology therapies may avoid in-person pharmacy visits due to stigma or logistical challenges.
DTP dispensing supports these needs through:
Discreet home delivery
Adherence tools and pharmacist check-ins
Secure handling designed for specialty medications
By combining discreet delivery, clinical support, and reliable cold-chain control into a single, coordinated model, DTP creates a private, safe, and patient-centered pathway for individuals who depend on specialty therapies.
Benefits of DTP Dispensing for Patients & the Healthcare System
The advantages of DTP dispensing extend beyond individual patient convenience to create systemic improvements in healthcare delivery.
Faster Therapy Initiation
Clinical evidence consistently demonstrates that rapid treatment initiation improves outcomes. For HIV patients, same-day antiretroviral therapy initiation has been linked to improved viral suppression and lower mortality rates. In rheumatoid arthritis patients, early initiation of disease-modifying therapy is associated with higher remission rates.
DTP dispensing accelerates time to therapy by eliminating the handoffs and delays inherent in traditional pharmacy workflows. When prescription, verification, fulfillment, and delivery operate as a single coordinated process, patients start treatment faster.
Improved Medication Adherence
Adherence requires more than just filling a prescription. It requires patients to actually take their medications as directed over time. DTP dispensing supports adherence through proactive refill reminders, regular check-ins, and streamlined reordering processes.
When patients know their medication will arrive reliably, without unexpected costs or administrative barriers, they're more likely to stay on therapy. The predictability that DTP dispensing provides creates conditions for sustained adherence.
Greater Transparency and Trust
Patients deserve to know what their medications will cost before they commit to therapy. DTP dispensing models that surface pricing information at the point of prescribing rather than at the pharmacy counter build trust between patients and their care teams.
Recent regulatory changes have prioritized prescription drug price transparency, requiring health plans to provide personalized cost-sharing estimates. DTP dispensing platforms are well-positioned to deliver this transparency, helping patients make informed decisions about their treatment options.
Visualizing the DTP Dispensing Journey
After exploring the challenges and benefits of direct‑to‑patient dispensing, it helps to see how the workflow comes together. The illustration below summarises the DTP dispensing process from prescription to delivery:
Prescribing: the clinician sends a prescription.
Coverage and affordability checks: automated coverage checks, benefits investigation and affordability support occur up front.
Medication fulfillment: once coverage is confirmed, the medication is prepared and ready for delivery.
Home delivery: the medication is shipped directly to the patient, closing the loop.
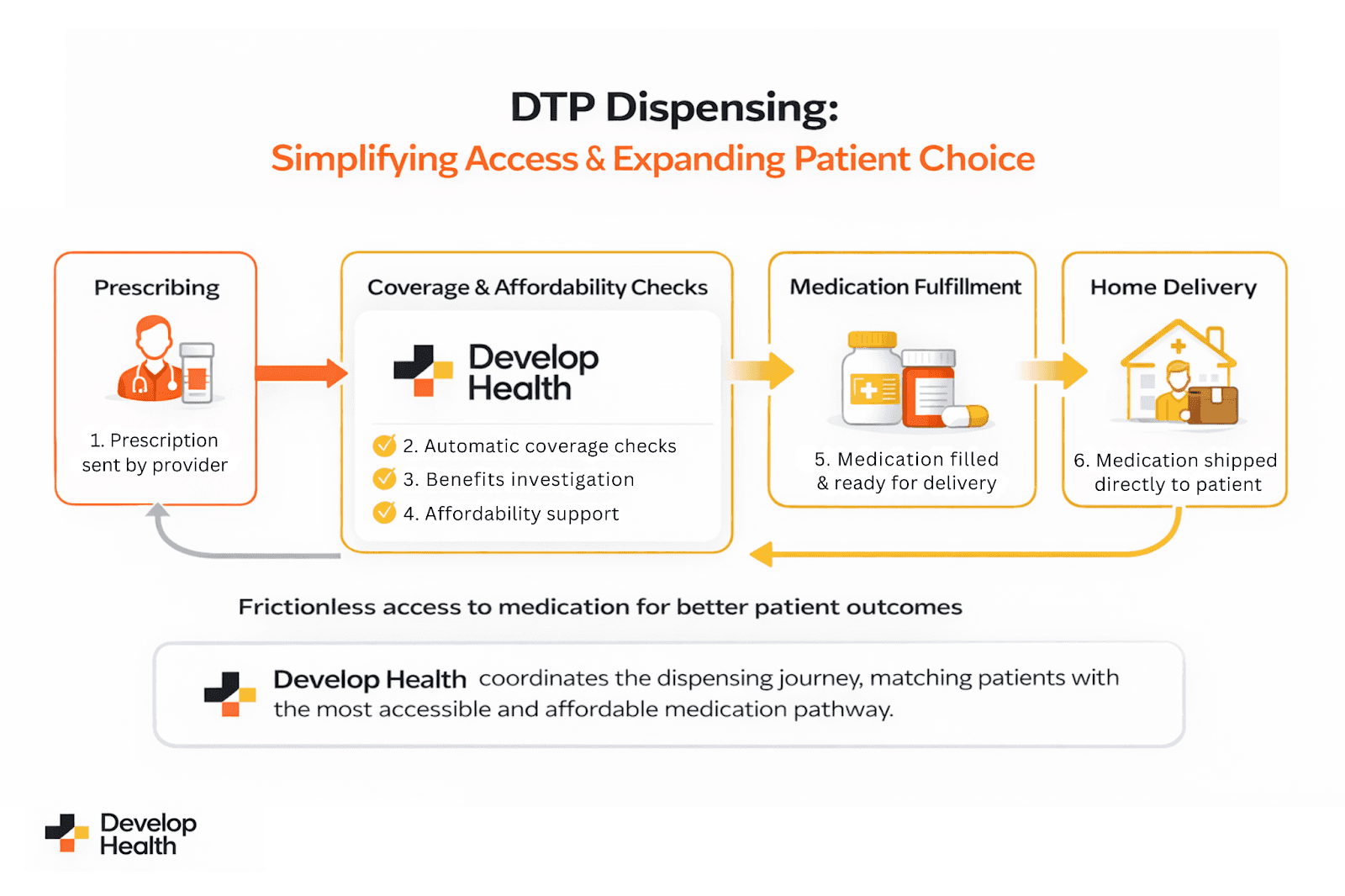
(Caption Here)
A prescription triggers automatic coverage and affordability checks, followed by medication fulfillment, leading to direct home delivery. Develop Health coordinates each step, making medication access faster, more transparent and patient‑centered.
[Technical SEO Alt text]: Flow diagram of the Direct‑to‑Patient (DTP) dispensing process, illustrating steps from prescribing to automatic coverage and affordability checks, medication fulfillment and home delivery by Develop Health.
DTP Dispensing Within the Broader Enablement Framework
DTP dispensing is one component of a broader direct-to-patient enablement model that integrates:
Benefit verification
Prior authorization automation
Affordability program navigation
Fulfillment and cold-chain logistics
Delivery and ongoing patient support
Unlike a simple mail-order pharmacy, DTP manages the entire access and support journey, anticipating barriers and guiding patients through the best pathway for their individual needs.
From Prescription to Possibility
DTP dispensing represents a fundamental shift in how patients access medications, one that prioritizes clarity, coordination and choice over fragmentation and delay. DTP removes barriers that have long disrupted therapy initiation and adherence.
As medication access grows more complex, models that simplify the journey will define the future of care delivery. DTP dispensing doesn’t replace existing pharmacy channels; it strengthens the system by ensuring patients reach treatment faster, with greater transparency, confidence and continuity of care.
Frequently Asked Questions (FAQs)
How does DTP dispensing protect patient data and privacy?
DTP dispensing protects patient data through secure digital workflows, encrypted communication, and compliance with all HIPAA requirements. Additionally, it limits external handoffs, reducing exposure to data breaches. As a result, patients have a protected, confidential access pathway, especially important for sensitive conditions that require discretion.
Can DTP dispensing integrate with electronic health record (EHR) systems?
Yes. Modern DTP platforms integrate directly with EHR systems to streamline prescribing, surface real-time coverage details, and automate benefit verification. This integration reduces manual tasks for providers and ensures patients move quickly from prescription to fulfillment without administrative delays or repeated coordination.
How does DTP dispensing handle urgent or time-sensitive medication needs?
DTP dispensing accelerates urgent therapy starts through automated BV/PA, real-time cost checks, and rapid fulfillment workflows. Expedited shipping options and coordinated clinical review ensure that critical medications reach patients quickly. Consequently, individuals with time-sensitive conditions avoid delays common in traditional pharmacy channels.
Does DTP dispensing support multilingual or low-literacy patient populations?
Yes. DTP models offer multilingual communication, simplified instructions, and guided support to help patients navigate insurance, affordability programs, and refills. These features remove barriers created by limited health literacy and ensure patients understand each step, thereby improving access and adherence.
How do healthcare providers benefit from DTP dispensing?
Providers benefit through reduced administrative workload, fewer coverage-related callbacks, and improved visibility into a patient’s access status. Additionally, automated processes for PA and BV shorten turnaround times, allowing clinicians to deliver timely care. This coordinated model strengthens continuity and enhances provider-patient trust.
Sources
Share this article
Nicolas Kernick is Head of Growth and Operations at Develop Health, where he helps scale Al-driven solutions that streamline medication access and transform clinical workflows. He worked across the US and Europe for 10 years at BCG before leaving to join a tech startup called SandboxAQ. He holds a First Class Degree in Physics from the University of Cambridge and was a Baker Scholar at Harvard Business School. With a deep interest in healthcare innovation and technology, Nicolas writes about how Al can improve patient outcomes and reduce administrative burden across the heathcare ecosystem.








